The human microbiome, a complex ecosystem of microorganisms living in and on the body, plays a pivotal role in maintaining health and influencing disease. Gut bacteria, in particular, have been linked to a wide array of conditions, from metabolic disorders to immune system dysfunctions. Research has begun to unravel how these microscopic inhabitants can sway health outcomes, signaling a paradigm shift in the understanding of disease pathology. This exploration delves into seven diseases that may originate from imbalances within the gut microbiota, highlighting the intricate relationship between these organisms and human health.
Contents
Obesity

The connection between gut microbiota and obesity is a focus of increasing scientific inquiry. Studies suggest that individuals with a diverse microbiome are less likely to suffer from obesity compared to those with less microbial variety. These microbes impact fat storage and energy regulation, potentially influencing body weight. Factors such as diet, antibiotic use, and lifestyle can significantly alter the gut ecosystem, thereby affecting obesity risk.
Modifications in diet can reshape the gut microbiome, offering a pathway to combat obesity. High-fiber foods, for instance, promote the growth of beneficial bacteria that are associated with weight management. Conversely, diets high in processed foods and sugars can lead to a less diverse gut flora, contributing to weight gain. Understanding the diet-microbiome relationship opens up possibilities for targeted nutritional interventions to prevent and treat obesity.
Type 2 Diabetes

The gut microbiota plays a critical role in the development of type 2 diabetes by influencing insulin resistance. Research indicates distinct differences in the microbiomes of individuals with diabetes compared to healthy controls, suggesting a direct link. These microbial communities can affect the host’s metabolism, immune function, and even the integrity of the gut barrier, all of which are factors in insulin sensitivity.
Emerging therapies that target the gut microbiota, including the use of probiotics and prebiotics, show promise in improving glucose metabolism. These interventions aim to restore a healthy balance of gut bacteria, potentially reducing insulin resistance and mitigating the risk of type 2 diabetes. Clinical trials continue to explore the efficacy of these microbiota-based treatments, offering hope for a novel approach to managing this chronic disease.
Inflammatory Bowel Disease (IBD)
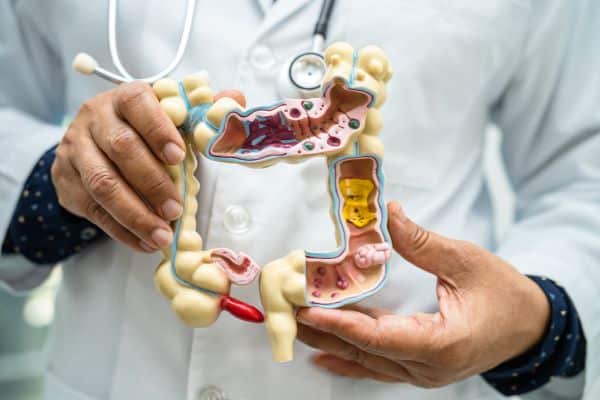
Inflammatory Bowel Disease, encompassing conditions such as Crohn’s disease and ulcerative colitis, is increasingly linked to imbalances in gut bacteria. The disruption of the normal microbiota can lead to an inappropriate immune response, triggering inflammation in the gastrointestinal tract. This suggests that managing gut bacteria could be a key strategy in treating and preventing IBD.
Research into microbiota-based therapies for IBD is burgeoning, with some studies showing promise in using fecal microbiota transplants (FMT) to restore healthy microbial communities in the gut. This approach, alongside other emerging treatments aimed at modulating the gut microbiome, points to a future where IBD management may become highly personalized, based on individual microbiome profiles.
Irritable Bowel Syndrome (IBS)
Evidence increasingly supports the role of gut microbiota dysbiosis in the pathogenesis of Irritable Bowel Syndrome (IBS). This condition, characterized by symptoms such as bloating, gas, and abdominal pain, affects millions worldwide. Alterations in the composition and function of the gut bacteria have been associated with the severity of IBS symptoms, suggesting a direct link between gut health and IBS. Studies have found that individuals with IBS often have lower microbial diversity, which can exacerbate gastrointestinal discomfort.
Dietary modifications and the use of probiotic supplements are common strategies to manage IBS symptoms through the modulation of gut bacteria. Foods rich in probiotics, such as yogurt and fermented foods, can help to increase the abundance of beneficial gut bacteria, offering relief from some IBS symptoms. Additionally, diets low in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) have been shown to reduce bloating and discomfort in many IBS sufferers. These approaches highlight the importance of gut microbiota in the management of IBS and underscore the potential for dietary interventions to improve quality of life for those affected.
Cardiovascular Disease

Gut bacteria play a surprising role in the development of cardiovascular disease by metabolizing dietary nutrients like choline and L-carnitine into trimethylamine N-oxide (TMAO), a compound linked to heart disease. This process illustrates the indirect ways in which the gut microbiome can influence heart health. Furthermore, research has indicated that people with certain microbiota profiles may have an increased risk of developing cardiovascular conditions, suggesting the potential for gut bacteria to serve as biomarkers for heart disease risk.
The exploration of microbiota-targeted therapies offers exciting prospects for cardiovascular disease prevention and treatment. By manipulating the gut microbiome, it may be possible to reduce the production of harmful metabolites like TMAO. Probiotic and prebiotic interventions, along with dietary adjustments, are under investigation for their potential to positively influence heart health. These findings underscore the complexity of the relationship between the gut microbiome and cardiovascular disease, opening new avenues for research and therapy.
Anxiety And Depression

The gut-brain axis represents a complex communication network through which the gut microbiota can exert significant effects on mental health, including conditions like anxiety and depression. This connection is supported by a growing body of research suggesting that the composition of the gut microbiota can influence brain chemistry and, consequently, emotions and behavior. Dysbiosis has been linked to increased levels of stress, anxiety, and depression, highlighting the potential for gut microbiota modulation as a therapeutic strategy.
Studies on probiotics, or psychobiotics, have begun to reveal potential benefits for mental health by altering gut bacteria. These beneficial microbes may improve mood and cognitive function by producing neurotransmitters like serotonin and dopamine, or by modulating the immune system to reduce inflammation, a known factor in some mood disorders. While research in this area is still emerging, the potential for probiotics to contribute to the treatment of anxiety and depression is a compelling aspect of the gut-brain connection.
Autoimmune Diseases

Emerging research suggests that dysbiosis, or an imbalance in gut microbiota, may contribute to the onset and progression of autoimmune diseases. By affecting immune tolerance and promoting inflammation, altered gut bacteria can play a role in the body’s immune system mistakenly attacking its own tissues. This connection has sparked interest in the gut microbiome as a potential target for therapeutic interventions in conditions like rheumatoid arthritis and multiple sclerosis.
The role of the gut microbiome in specific autoimmune diseases is an area of intense study, with the goal of developing new treatments that restore microbial balance. For instance, dietary interventions, probiotics, and fecal microbiota transplants are being explored for their ability to modulate the immune response and reduce autoimmune symptoms. These approaches offer hope for more personalized and effective treatments, emphasizing the importance of the gut microbiome in autoimmune disease management.
The Bottom Line
The intricate relationship between gut bacteria and human health extends far beyond digestion, influencing everything from metabolism to mental well-being. The evidence linking gut microbiota imbalances to a range of diseases underscores the potential of microbiome-targeted therapies. As research progresses, the goal is to harness this knowledge to prevent and treat conditions associated with dysbiosis. Embracing a lifestyle that promotes a healthy gut microbiome—through diet, exercise, and possibly probiotic supplementation—may be key to mitigating the risk of these diseases. In doing so, the focus shifts towards a more holistic approach to health, recognizing the gut microbiome as a central factor in the quest for well-being.


