Body Mass Index (BMI) has long been a staple in health assessments worldwide, serving as a quick reference for categorizing individuals into various weight categories. Initially developed in the early 19th century, BMI is widely used by medical professionals and health organizations to gauge health risks associated with weight. Despite its widespread use, the reliability and effectiveness of BMI as a health indicator are subjects of ongoing debate. This post delves into the history, application, and criticisms of BMI, exploring its role in individual and public health and questioning its status as a reliable health indicator.
Contents
History and Development of BMI

BMI, or Body Mass Index, was conceived by Adolphe Quetelet during the 19th century. It was originally termed the Quetelet Index, designed to provide a simple means to classify sedentary individuals’ body weight relative to their height. Throughout the years, BMI gained prominence as a straightforward tool for epidemiologists to understand and manage population health, particularly in identifying trends in obesity. It became a crucial tool in the burgeoning field of public health, guiding policies and interventions.
As BMI embedded itself into clinical practice and public health policy, its use expanded from a general population assessment tool to an individual health indicator. Despite its initial non-clinical beginnings, BMI’s ease of calculation and universal applicability made it a standard fixture in health assessments, leading to its current role in medical screenings, insurance evaluations, and health education. Its enduring legacy and widespread acceptance have made it synonymous with health measurement despite emerging criticisms and challenges to its validity.
Understanding BMI Calculations
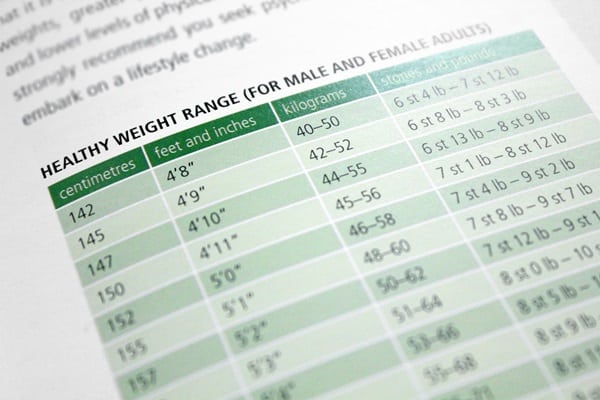
BMI is calculated by dividing an individual’s weight in kilograms by the square of their height in meters. This simple formula categorizes individuals into various groups, such as underweight, normal weight, overweight, and obese. These categories are based on established ranges, aiming to provide a quick assessment of potential health risks related to body size. The simplicity of this calculation has made BMI a universally recognized and easily applicable health metric.
However, while BMI provides a quick metric, its simplicity overlooks factors like muscle mass, bone density, overall body composition, and racial and sex differences. These limitations can lead to misleading categorizations, particularly for athletes with high muscle mass or individuals with denser bone structures. Consequently, the BMI can sometimes inaccurately reflect an individual’s health status or risk factors. Critics argue for the adoption of more comprehensive measures that account for a wider array of body types and health markers.
BMI as a Health Predictor

BMI is commonly used as a predictor for a range of health conditions, including heart disease, diabetes, and various forms of cancer. Its widespread application in clinical settings is largely due to its correlation with these adverse health outcomes. Higher BMI levels are typically associated with an increased risk of chronic diseases and health issues related to overweight and obesity. It serves as a starting point for many health discussions and interventions.
However, while a high BMI can indicate risk for various health conditions, it doesn’t directly measure health or fat distribution. This means that two individuals with the same BMI might have vastly different health profiles and risks. As such, reliance solely on BMI overlooks the complex interplay of genetic, lifestyle, and environmental factors contributing to an individual’s health. This has led to calls for more personalized health assessments, integrating BMI with other health indicators for a fuller picture.
Criticisms of BMI

One of the primary criticisms of BMI is its oversimplification of body weight and its disregard for muscle and bone mass. It doesn’t differentiate between muscle and fat, leading to potentially misleading categorizations of individuals, especially those who are particularly muscular or have less muscle mass. This can result in the mislabeling of healthy, fit individuals as overweight or obese and vice versa. This oversimplification is a significant flaw in its application as a universal health indicator.
Furthermore, BMI’s one-size-fits-all approach has been questioned for its applicability across different ethnicities and age groups. Different populations have varying body compositions and health implications associated with weight, making the universal application of BMI problematic. As such, critics argue for a more nuanced approach to health assessment, one that takes into account the diverse nature of human bodies and the multifaceted aspects of health. The need for more culturally and individually sensitive health metrics is increasingly recognized in the medical and public health communities.
BMI and Public Health Policy

BMI’s influence extends beyond individual health assessments into the realm of public health policy. Governments and health organizations often use BMI as a benchmark to identify at-risk populations, allocate resources, and formulate health promotion strategies. It has become a tool for shaping policies aimed at combating obesity and associated health conditions, influencing everything from nutritional guidelines to fitness campaigns. The simplicity and cost-effectiveness of BMI make it an attractive option for large-scale health initiatives.
However, the reliance on BMI in public health policy has also attracted criticism. Critics argue that it can lead to oversimplified approaches to complex health issues, potentially stigmatizing individuals and overlooking the multifaceted nature of health and wellness. There are concerns about the effectiveness of BMI-centric policies in actually improving health outcomes, prompting a reevaluation of how best to use and interpret BMI in the public health sphere. The challenge lies in balancing the practical utility of BMI with a more nuanced understanding of health and disease.
Alternatives to BMI

As the limitations of BMI become more widely recognized, there’s increasing interest in alternative health and fitness measures. Body fat percentage, waist-to-hip ratio, and waist circumference are just a few of the metrics gaining attention. These alternatives often provide a more nuanced view of body composition and health, accounting for factors like muscle mass, fat distribution, and other individual variations. They are heralded as potentially more accurate indicators of health risks associated with body size and composition.
Despite the promise of these alternative metrics, they also come with their own set of challenges. Issues such as measurement complexity, standardization, and accessibility can hinder their widespread adoption. Additionally, like BMI, no single metric perfectly captures an individual’s health status, and each has its own limitations and biases. The debate continues on how to best integrate these alternatives into clinical practice and public health, aiming for a more holistic and personalized approach to health assessment.
Societal and Cultural Perceptions of BMI

BMI is more than a health metric; it’s a cultural symbol that influences societal perceptions of health, beauty, and normalcy. In many cultures, BMI categories have become synonymous with labels of ‘underweight,’ ‘normal,’ ‘overweight,’ and ‘obese,’ carrying significant social and psychological implications. These labels can affect individual self-esteem, body image, and even the way people are treated by society and within healthcare settings. The cultural prominence of BMI shapes attitudes toward body size and health, often in ways that oversimplify complex realities.
In addition, the cultural critique of BMI highlights how it can reinforce or challenge prevailing beauty standards and stigmas associated with body size. In some societies, a low BMI is idealized, while in others, a more robust body is celebrated. These cultural nuances underscore the importance of contextualizing BMI within broader societal values and norms. Recognizing the cultural dimension of BMI is crucial for understanding its impact on individual and collective health perceptions and for promoting health and wellness in a culturally competent manner.
Embrace a Comprehensive Approach to Health
As you reflect on the limitations and applications of the Body Mass Index, it’s clear that a singular focus on BMI is insufficient for comprehensive health assessment. You are encouraged to consider a variety of factors, including alternative health indicators and personal context when evaluating health and making lifestyle decisions. Let’s advocate for a more nuanced, personalized approach to health that recognizes the complexity of individual bodies and encourages a broader understanding and application of health metrics in both personal and public realms.


